Volume 18, Issue 3 (May-Jun 2024)
mljgoums 2024, 18(3): 29-31 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Baniaghil S S, Balochi F, Ahmadi A. Evaluation prevalence of Rh system major antigens (D, C, c, E, e) and their phenotypes in blood donors of Golestan province, Iran. mljgoums 2024; 18 (3) :29-31
URL: http://mlj.goums.ac.ir/article-1-1595-en.html
URL: http://mlj.goums.ac.ir/article-1-1595-en.html
1- Blood Transfusion Research Center, High Institute for Research and Education in Transfusion Medicine, Tehran, Iran
2- Laboratory Science Research Center, Golestan University of Medical Sciences, Golestan, Iran ,drahmadi@goums.ac.ir
2- Laboratory Science Research Center, Golestan University of Medical Sciences, Golestan, Iran ,
Full-Text [PDF 402 kb]
(1320 Downloads)
| Abstract (HTML) (3463 Views)
Full-Text: (791 Views)
Introduction
Blood groups are determined by inherited characteristics of red blood cell (RBC) membrane antigens. Blood group systems consist of one or more antigens produced by one or more closely related genes. The International Society of Blood Transfusion has identified 43 blood group systems and more than 300 RBC antigens (1,2). The Rh blood group system is the second most important blood group system, after the ABO system, and consists of 50 defined blood group antigens. Among these, the five most important antigens are D, C, c, E, and e (3).
Antigen D is the most immunogenic of these antigens. The clinical significance of these antigens lies in the fact that if a person lacks one or more antigens and receives RBCs containing those antigens, antibodies are likely to be produced against them, leading to alloimmunization and hemolytic reactions. The group most at risk of these problems is multitransfused patients (4). Determining Rh phenotypes can play a crucial role in preventing alloimmunization in multitransfusion cases. In most blood banks, only the ABO and RhD blood group systems are matched for blood donors and recipients when RBCs are transfused (5). The rate of alloimmunization, or the production of antibodies that may potentially destroy foreign or donor RBCs, is significantly higher (8-76%) among patients receiving multitransfusions, such as those with sickle cell disease and thalassemia, and it increases with repeated transfusions (6). In countries where phenotyping is mandatory, such as France since 2002, post-transfusion alloimmunization has become rare (7).
A healthy and compatible blood supply is a critical issue for blood banks and hospitals, especially for patients with thalassemia major. Therefore, this study investigated the frequency and prevalence of major Rh blood group antigens in donors to provide healthy and compatible blood for recipients and reduce the incidence of alloimmunization and hemolytic reactions. This is the first step in determining the frequency of these antigens in the donor population and in creating a bank of negative antigen cells.
Methods
A descriptive study was conducted on 576 healthy blood donors (269 Turkmen and 306 Fars) with a 95% confidence level from June 2020 to July 2021 at the Golestan Blood Bank. Each donor was considered only once. The age of the blood donors ranged from 20 to 50 years, with an average age of 33 ± 7.7 years.
For antigen typing, a 6 mL blood sample was collected at the time of donation through the diversion pouch into a tube containing ethylenediaminetetraacetic acid. All collected blood units were phenotyped for the major Rh antigens (D, C, c, E, e). Units that tested positive for the Rh D antigen were labeled as Rh-positive. Units that tested negative for the Rh D antigen were further tested for weak expression of the D antigen. The pattern of reactions was evaluated, and based on the agglutination or non-agglutination of globular samples with antisera, the phenotype of each sample was determined.
For statistical analysis, data were analyzed using SPSS for Windows version 19. The frequencies of Rh antigens and phenotypes were calculated by dividing the number of samples with positive results by the total number of samples. Chi-square values were calculated to compare the frequency of antigens and the distribution of haplotypes between different ethnic groups. A p-value < 0.05 was considered significant. The findings of this study were also compared with similar studies conducted in other regions.
Results
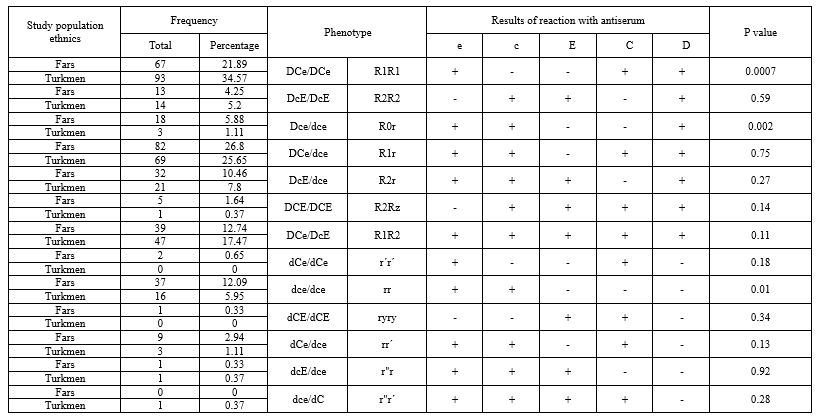
A total of 575 blood donors were included in the study, and their blood samples were typed for antigens in the major Rh blood group system. The study included donors aged 20 to 50 years, with an average age of 33 ± 7.7 years. For the Rh blood group system, all samples were typed for the antigens D, C, E, c, and e. RhD typing, along with typing for other major Rh antigens, was performed on all donors. Of the samples, 87.76% were D positive and 12.24% were D negative. Among the five major antigens, the e antigen was found to be the most common at 93.59%, followed by C (73.6%), c (72.1%), and E (30.83%), which was the least common (Table 1). The most common phenotype observed was R1R1 followed by R1r and R1R2 among the total study population. The most common phenotype among Rh-positives was R1R1, while among Rh negatives it was rr. There were significant differences in the frequencies of the R1R1 (P-value = 0.0007), R0r (P-value = 0.002), and rr (P-value = 0.01) phenotypes between the Turkmen and Fars donors (Table 2).
The lowest frequencies of phenotypes in Rh-positive and Rh-negative donors were associated with R2Rz and r''r', and r"r and ryry, respectively (Table 3). The phenotype r"r´ was not detected in the Fars donors, and the phenotype r´r´ and ryry were not identified in the Turkmen donors.
Discussion
Although blood transfusions can save lives, they are not without risk. The immune system may produce alloantibodies when exposed to incompatible RBCs, and these antibodies can then bind to donor cells, leading to hemolytic transfusion reactions. Patients with Rh alloantibodies should receive blood that lacks these antigens. This requires the determination of the immunological characteristics of both blood products and recipients through immunohematology analyses, such as phenotyping in the Rh blood group system.
Rh system antibodies play a crucial role in blood transfusion. The production of alloantibodies against foreign antigens can cause a range of reactions, from mild to severe, including hemolytic disease in the fetus and infant, as well as hemolytic reactions following blood transfusions (8).
In this study, 87.76% of donors (Fars and Turkmen) were Rh-positive, similar to findings in Isfahan (9), the white population (10), and Morocco (11).
Among the other Rh antigens (C, c, E, e), the e and C antigens had the highest frequencies, at 93.59% and 73.6%, respectively. The frequency of the e antigen aligns with studies in Isfahan (9), Khorramabad (12), and China (13), while the frequency of the C antigen is consistent with studies from northeastern Iran (14), Khorramabad (12) and Iraqi Kurdistan (15). Compared to other regions, the highest frequency of the e antigen was observed in Morocco and India, while the highest frequency of the C antigen was found in China and Pakistan (Table 1). The E antigen had the lowest frequency at 30.83%, which is consistent with studies from northeastern Iran (14), Isfahan (9), and Iraqi Kurdistan (15) (Table 1).
The most common phenotypes among Rh-positive donors in this study were R1R1 (28.23%) and R1r (26.22%), respectively, similar to results from studies in northeastern Iran (14), Khorramabad (13), and Isfahan (10). Among Rh-negative donors, the most common phenotype was rr (9.02%), which is consistent with findings from northeastern Iran (14), Isfahan (9), and Iraqi Kurdistan (15). The lowest frequencies were observed for the R2Rz (1%) and ryry (0.33%) phenotypes in Rh-positive and Rh-negative donors, respectively. The r'r" phenotype was not detected in the Fars donors, which is similar to the results from northeastern Iran (14). Moreover, the r´r´ and ryry phenotypes were not identified in the Turkmen donors (Tables 2 and 3). These findings suggest that the frequency of Rh system antigens and phenotypes varies across different geographical regions, highlighting the need for independent studies in each region. ABO and Rh(D) blood types are routinely tested at blood transfusion centers, the other four Rh antigens (C, c, E, e) are not. This gap means that if a recipient lacks one of these antigens, there is a risk of alloimmunization. This study was an initial effort to identify the major Rh blood group system among blood donors in Golestan Province to enhance healthcare services and better serve patients.
Conclusion
Outcomes of such studies can be used to determine the prevalence of antigens in each region, manage blood consumption, organize negative antigen blood units, maintain existing blood reserves, reduce blood transfusion reactions, minimize alloimmunization, and identify rare phenotypes.
Acknowledgement
The authors would like to thank all the participants for their collaboration.
Funding sources
This study did not receive any grants from funding agencies, whether public, commercial, or non-profit.
Ethical statement
All stages of the implementation of this study were carried out according to the instructions of the Iranian Blood Transfusion Organization. Ethics approvals and consent to participate were not applicable.
Conflicts of interest
The authors declare that there are no conflicts of interest.
Author contributions
All authors contributed to one or more aspects of the study.
Blood groups are determined by inherited characteristics of red blood cell (RBC) membrane antigens. Blood group systems consist of one or more antigens produced by one or more closely related genes. The International Society of Blood Transfusion has identified 43 blood group systems and more than 300 RBC antigens (1,2). The Rh blood group system is the second most important blood group system, after the ABO system, and consists of 50 defined blood group antigens. Among these, the five most important antigens are D, C, c, E, and e (3).
Antigen D is the most immunogenic of these antigens. The clinical significance of these antigens lies in the fact that if a person lacks one or more antigens and receives RBCs containing those antigens, antibodies are likely to be produced against them, leading to alloimmunization and hemolytic reactions. The group most at risk of these problems is multitransfused patients (4). Determining Rh phenotypes can play a crucial role in preventing alloimmunization in multitransfusion cases. In most blood banks, only the ABO and RhD blood group systems are matched for blood donors and recipients when RBCs are transfused (5). The rate of alloimmunization, or the production of antibodies that may potentially destroy foreign or donor RBCs, is significantly higher (8-76%) among patients receiving multitransfusions, such as those with sickle cell disease and thalassemia, and it increases with repeated transfusions (6). In countries where phenotyping is mandatory, such as France since 2002, post-transfusion alloimmunization has become rare (7).
A healthy and compatible blood supply is a critical issue for blood banks and hospitals, especially for patients with thalassemia major. Therefore, this study investigated the frequency and prevalence of major Rh blood group antigens in donors to provide healthy and compatible blood for recipients and reduce the incidence of alloimmunization and hemolytic reactions. This is the first step in determining the frequency of these antigens in the donor population and in creating a bank of negative antigen cells.
Methods
A descriptive study was conducted on 576 healthy blood donors (269 Turkmen and 306 Fars) with a 95% confidence level from June 2020 to July 2021 at the Golestan Blood Bank. Each donor was considered only once. The age of the blood donors ranged from 20 to 50 years, with an average age of 33 ± 7.7 years.
For antigen typing, a 6 mL blood sample was collected at the time of donation through the diversion pouch into a tube containing ethylenediaminetetraacetic acid. All collected blood units were phenotyped for the major Rh antigens (D, C, c, E, e). Units that tested positive for the Rh D antigen were labeled as Rh-positive. Units that tested negative for the Rh D antigen were further tested for weak expression of the D antigen. The pattern of reactions was evaluated, and based on the agglutination or non-agglutination of globular samples with antisera, the phenotype of each sample was determined.
For statistical analysis, data were analyzed using SPSS for Windows version 19. The frequencies of Rh antigens and phenotypes were calculated by dividing the number of samples with positive results by the total number of samples. Chi-square values were calculated to compare the frequency of antigens and the distribution of haplotypes between different ethnic groups. A p-value < 0.05 was considered significant. The findings of this study were also compared with similar studies conducted in other regions.
Results
A total of 575 blood donors were included in the study, and their blood samples were typed for antigens in the major Rh blood group system. The study included donors aged 20 to 50 years, with an average age of 33 ± 7.7 years. For the Rh blood group system, all samples were typed for the antigens D, C, E, c, and e. RhD typing, along with typing for other major Rh antigens, was performed on all donors. Of the samples, 87.76% were D positive and 12.24% were D negative. Among the five major antigens, the e antigen was found to be the most common at 93.59%, followed by C (73.6%), c (72.1%), and E (30.83%), which was the least common (Table 1). The most common phenotype observed was R1R1 followed by R1r and R1R2 among the total study population. The most common phenotype among Rh-positives was R1R1, while among Rh negatives it was rr. There were significant differences in the frequencies of the R1R1 (P-value = 0.0007), R0r (P-value = 0.002), and rr (P-value = 0.01) phenotypes between the Turkmen and Fars donors (Table 2).
|
Table 1. Frequency of rh antigens based on serological response in the population of the present study and other studies
 |
Discussion
Although blood transfusions can save lives, they are not without risk. The immune system may produce alloantibodies when exposed to incompatible RBCs, and these antibodies can then bind to donor cells, leading to hemolytic transfusion reactions. Patients with Rh alloantibodies should receive blood that lacks these antigens. This requires the determination of the immunological characteristics of both blood products and recipients through immunohematology analyses, such as phenotyping in the Rh blood group system.
Rh system antibodies play a crucial role in blood transfusion. The production of alloantibodies against foreign antigens can cause a range of reactions, from mild to severe, including hemolytic disease in the fetus and infant, as well as hemolytic reactions following blood transfusions (8).
In this study, 87.76% of donors (Fars and Turkmen) were Rh-positive, similar to findings in Isfahan (9), the white population (10), and Morocco (11).
Among the other Rh antigens (C, c, E, e), the e and C antigens had the highest frequencies, at 93.59% and 73.6%, respectively. The frequency of the e antigen aligns with studies in Isfahan (9), Khorramabad (12), and China (13), while the frequency of the C antigen is consistent with studies from northeastern Iran (14), Khorramabad (12) and Iraqi Kurdistan (15). Compared to other regions, the highest frequency of the e antigen was observed in Morocco and India, while the highest frequency of the C antigen was found in China and Pakistan (Table 1). The E antigen had the lowest frequency at 30.83%, which is consistent with studies from northeastern Iran (14), Isfahan (9), and Iraqi Kurdistan (15) (Table 1).
The most common phenotypes among Rh-positive donors in this study were R1R1 (28.23%) and R1r (26.22%), respectively, similar to results from studies in northeastern Iran (14), Khorramabad (13), and Isfahan (10). Among Rh-negative donors, the most common phenotype was rr (9.02%), which is consistent with findings from northeastern Iran (14), Isfahan (9), and Iraqi Kurdistan (15). The lowest frequencies were observed for the R2Rz (1%) and ryry (0.33%) phenotypes in Rh-positive and Rh-negative donors, respectively. The r'r" phenotype was not detected in the Fars donors, which is similar to the results from northeastern Iran (14). Moreover, the r´r´ and ryry phenotypes were not identified in the Turkmen donors (Tables 2 and 3). These findings suggest that the frequency of Rh system antigens and phenotypes varies across different geographical regions, highlighting the need for independent studies in each region. ABO and Rh(D) blood types are routinely tested at blood transfusion centers, the other four Rh antigens (C, c, E, e) are not. This gap means that if a recipient lacks one of these antigens, there is a risk of alloimmunization. This study was an initial effort to identify the major Rh blood group system among blood donors in Golestan Province to enhance healthcare services and better serve patients.
Conclusion
Outcomes of such studies can be used to determine the prevalence of antigens in each region, manage blood consumption, organize negative antigen blood units, maintain existing blood reserves, reduce blood transfusion reactions, minimize alloimmunization, and identify rare phenotypes.
Acknowledgement
The authors would like to thank all the participants for their collaboration.
Funding sources
This study did not receive any grants from funding agencies, whether public, commercial, or non-profit.
Ethical statement
All stages of the implementation of this study were carried out according to the instructions of the Iranian Blood Transfusion Organization. Ethics approvals and consent to participate were not applicable.
Conflicts of interest
The authors declare that there are no conflicts of interest.
Author contributions
All authors contributed to one or more aspects of the study.
Research Article: Research Article |
Subject:
Immunology
Received: 2022/11/12 | Accepted: 2023/04/11 | Published: 2024/06/3 | ePublished: 2024/06/3
Received: 2022/11/12 | Accepted: 2023/04/11 | Published: 2024/06/3 | ePublished: 2024/06/3
References
1. de Mattos LC. Structural diversity and biological importance of ABO, H, Lewis and secretor histo-blood group carbohydrates. Rev Bras Hematol Hemoter 2016; 38: 331-40. [View at Publisher] [DOI] [PMID] [Google Scholar]
2. ISBT. 202 Table of blood group antigens within systems. 2021. [View at Publisher]
3. McPherson RA, Pincus MR. Henry's Clinical Diagnosis and Management by Laboratory Methods. 23rd ed. St. Louis, Missouri: Elsevier. 2017; 687. [View at Publisher]
4. Fasano RM, Chou ST. Red blood cell antigen genotyping for sickle cell disease, thalassemia, and other transfusion complications. Transfus Med Rev 2016; 30(4): 197-201. [View at Publisher] [DOI] [PMID] [Google Scholar]
5. Kulkarni S, Choudhary B, Harita Gogri H, Jayashree Sharma J, Madkaikar M. Red cell antigen phenotypes in blood donors & thalassaemia patients for creation of red cell antigen-matched inventory. Indian J Med Res. 2020; 152(3): 273-279. [View at Publisher] [DOI] [PMID] [Google Scholar]
6. Chou ST, Liem RI, Thompson AA. Challenges of alloimmunization in patients with haemoglobinopathies. Br J Haematol. 2012; 159(4): 394-404. [View at Publisher] [DOI] [PMID] [Google Scholar]
7. Pachaury R, Arya D.R, Lai Mahawar N, Bharti A, Kumar Das P. Frequency of Rh Phenotypes in voluntary Blood Donors. JMSCR 2017: 05(07). 25083-88. [View at Publisher] [Google Scholar]
8. Flegel WA. The genetics of The Rhesus Blood Group System. Blood Transfuse. 2007; 5(2): 50-570. [View at Publisher] [PubMed] [Google Scholar]
9. Vahid Dastjerdi A, Salimi Sh, Jafarian M, Akbari N, Yavari F, Hashemi S.S. Phenotype determination of main Rh system antigens in the regular of Isfahan Blood Transfusion Center in 2016. Sci J Iran Blood Transfus Organ. 2018; 15(1): 12-20. [View at Publisher] [Google Scholar]
10. Reid ME, Lomas-Francis C, Olsson ML. The Blood group antigen facts book . 2nd ed. USA: Academic Press.2004.109-38. [View at Publisher] [DOI] [PMID] [Google Scholar]
11. Zahid H, Yahyaoui A, Uwingabiye J, EI Khazraji A, Labrini F, Hadef R, et al. Phenotype frequencies of Rh and Kell blood group systems in blood transfusion department of avicenna military hospital, Marracech, Morocco. International journal of Medicine & Health Research 2016; 2(1): 1-10. [View at Publisher] [Google Scholar]
12. Abdi J , Kiani AA. Seroepidemiologic evaluation of Rh System major antigens(D,C,E,c,e) and their phenotypes among the blood donors in Khorramabad , Iran. Sci J Iran Blood Transfus Organ. 2009 ; 6(3) : 219-26. [View at Publisher] [Google Scholar]
13. Yu Y, Ma C, Sun X, Guan X, Zhang X, Saldanha J, et al. Frequencies of red blood cell major blood group antigens and phenotypes in the Chinese Han population from Mainland. Int J Immunogenet. 2016; 43(4):226-35. [View at Publisher] [DOI] [PMID] [Google Scholar]
14. Keramati MR, Shakibaei H, Kheiyyami MI, Ayotollahi H, Badiei Z, et al. Blood group antigens frequencies in the northeast of Iran. Transfus Apher Sci. 2011; 45(2) : 133-136. [View at Publisher] [DOI] [PMID] [Google Scholar]
15. Getta HA, Amin SS, Khoshnaw N, Muhammad BA. Distribution of red cell antigens according to ABO, Rh and other rare blood group systems in Kurdish ethnicity. Iraqi Journal of Hematology. 2015; 1(5): 55-80. [View at Publisher] [DOI] [Google Scholar]
16. Moafi AR, Rahgozar S, Pourfathollah AA, Hariri MM. Blood group antigens frequency: a comparative study in intermediate thalassemics versus healthy people in Isfahan. Sci J Iran Blood Transfus Organ. 2005; 2(3): 23-29. [View at Publisher] [Google Scholar]
17. Mahmood R, Alam M, Altaf Ch, Abbasi AM, Malik HS. Phenotypic Profile of Rh Blood Group System among Females of Child-Bearing Age in Pakistan. Hematol Transfus Int J. 2018; 6(1): 1-4. [View at Publisher] [DOI] [Google Scholar]
18. Anwr N, Borhany M, Ansari S, Khurram S, Zaidi U, Nasser I, et al. Trands of ABO and Rh phenotypes in transfusion-dependent patients in Pakistan. Immunohematology. 2016; 32(4): 170-3. [View at Publisher] [DOI] [PubMed] [Google Scholar]
19. Makroo RN, Bhatia A, Gupta R, Phillip J. Prevalence of Rh, Duffy, Kell, Kidd & MNSs blood group antigens in the indian blood donor population .Indian J Med Res. 2013 ; 137(3) :521-26. [View at Publisher] [PubMed] [Google Scholar]
20. Kahar MA, Patel RD. Phenotype frequencies of blood group systems (Rh, Kell, Kidd, Duffy, MNS, P, Lewis, and Lutheran) in blood donors of south Gujarat, India. Asian J Transfus Sci. 2014; 8(1): 51-5. [View at Publisher] [DOI] [PMID] [Google Scholar]
21. Garg N, Sngh D.K, Tomar R, Singh B. Phenotype Prevalence of Blood Group System (ABO, Rh, Kell) in Voluntary, Healthy Donors-Experience of a Tertiary Care Hospital in Delhi,North India. J Blood Disord Transfus. 2015; 6(4): 1-4. [View at Publisher] [Google Scholar]
22. Philip CJ, Mallhi RS, Yadav CP Sarkar RS. Proportion of Rh phenotypes in voluntary blood donors. Med J Armed Force India. 2013; 330-334. [View at Publisher] [DOI] [PMID] [Google Scholar]
23. Chitra M, Jagannathan S.Y, Arumugan P, Ravishankar J. Prevalence of Rh Antigens among voluntary blood donors in Chennai , Tamil Nadu, India. Int J of Res in Med Sci. 2016; 4(12): 5360-5363. [View at Publisher] [DOI]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.