Volume 19, Issue 1 (Jan-Feb 2025)
mljgoums 2025, 19(1): 19-21 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Pol S, Shah P, Gaikwad V, Dharmshale S, Rajmane M, Karyakarte R. Impact of COVID-19 pandemic on tuberculosis. mljgoums 2025; 19 (1) :19-21
URL: http://mlj.goums.ac.ir/article-1-1843-en.html
URL: http://mlj.goums.ac.ir/article-1-1843-en.html
Sae Pol1 

 , Pooja Shah1
, Pooja Shah1 

 , Vaishali Gaikwad2
, Vaishali Gaikwad2 

 , Sujata Dharmshale3
, Sujata Dharmshale3 

 , Mansi Rajmane1
, Mansi Rajmane1 

 , Rajesh Karyakarte *4
, Rajesh Karyakarte *4 




 , Pooja Shah1
, Pooja Shah1 

 , Vaishali Gaikwad2
, Vaishali Gaikwad2 

 , Sujata Dharmshale3
, Sujata Dharmshale3 

 , Mansi Rajmane1
, Mansi Rajmane1 

 , Rajesh Karyakarte *4
, Rajesh Karyakarte *4 


1- Department of Microbiology, BJ Medical College, Pune, India
2- Department of Microbiology, Government Medical College, Satara, India
3- Department of Microbiology, Government Medical College, Baramati, India
4- Department of Microbiology, BJ Medical College, Pune, India ,karyakarte@hotmail.com
2- Department of Microbiology, Government Medical College, Satara, India
3- Department of Microbiology, Government Medical College, Baramati, India
4- Department of Microbiology, BJ Medical College, Pune, India ,
Full-Text [PDF 328 kb]
(679 Downloads)
| Abstract (HTML) (2371 Views)
Discussion
This study was conducted in a tertiary care hospital from 1st January 2018 to 31st December 2022. The total samples received for M. tuberculosis from 2018-2022 were 3543, 3823, 3682, 3248, and 3381 respectively. Samples positive for M. tuberculosis were 20.9%, 18.2%, 15.5%, 15.8%, and 16.8% from 2018 to 2022, respectively. The rifampicin resistance from 2018 to 2022 was found to be 11.0%, 9.8%, 7.3%, 6.4%, and 11.9%, respectively. During the study period, two years i.e., 2020 and 2021 were the COVID-19 pandemic period in India. Moreover, many restrictions were imposed to stop the spread of COVID-19 during these years, such as wearing masks, avoiding social gatherings, maintaining social distancing, etc., which are all isolation measures. It was observed that the positivity of TB in our tertiary care hospital decreased in 2020 and 2021. The rifampicin resistance also decreased during the same period.
In the present study, the years 2018 and 2019 can be considered the pre-COVID-19 period, while the year 2022 was considered the COVID-19 period without restrictions. M. tuberculosis positivity and rifampicin resistance were higher in the pre-COVID-19 (22.5%) and post-COVID-19 (16.8%) periods compared to the COVID-19 period with restrictions (15.7%). Tuberculosis and COVID-19 are diseases of the respiratory system and they spread through droplet nuclei (10). Isolation measures followed during COVID-19 might contribute to decreasing cases of TB during 2020 and 2021.
The importance of masks in the prevention of airborne diseases has been mentioned by CDC and Asadi et al. (11,12). Moreover, the lockdowns likely had a significant impact, as fear of COVID-19 led people to minimize contact even with family members. This reduction in interaction may have helped prevent the spread of infection within households and the broader community. Afterward, vaccination was introduced widely in India. In 2021, India reported around 1.6 lakhs vaccination every hour (12). At the same time, cases of COVID-19 started decreasing and restrictions were partially released. In 2022, the milder omicron wave was documented; however, strict restrictions were not imposed again. This could be the major reason for the increase in cases in 2022. In the study conducted by Miligori et al., TB decreased from 32,898 (Mean±SD=2742±177 per month) in 2019 to 16,396 (1366±308 per month; p<0.0001) in 2020, with a sudden decline in March 2020, concomitantly with the commencement of lockdown in the majority of the countries (13). This epidemiological change was observed in all countries, except TB centers in Australia, Singapore, and Virginia (13).
In the present study, the lowest rifampicin resistance was seen in 2021. The possible reason could be lockdown restricted movement of people and social gatherings. As a result, many people may not have accessed diagnostic facilities, leading to underreporting of rifampicin resistance. In the study conducted by Trajman A. et al., the COVID-19 pandemic had a sufficient impact on TB care cascade, resulting in decrease in TB testing and notifications of TB, primarily as a result of disrupted TB services and constrained patient movement (14). However, restrictions were released, and an increase was reported in rifampicin resistance in 2022.
Extrapulmonary TB-positive cases were not seen to decrease significantly during the COVID-19 period. In fact, we observed an increase in the number of TB-positive cases from extrapulmonary samples in 2021. This clearly indicates that wearing masks has prevented only pulmonary TB. As very few studies are available on TB in the COVID-19 period, we could not compare our results with similar studies.
In case of rifampicin-resistant TB, we could not track family members of rifampicin-resistant patients to confirm their rifampicin status. These findings cannot be generalized, since this is a single-center study. Further studies, especially in bigger institutes will enable us to know the overall status and can be useful to take further action. There is a need to conduct a cohort study on people who wear masks and those who do not.
Conclusion
Restrictions imposed during the COVID-19 period could have decreased TB as well as rifampicin resistance. There was not much difference in total sample size received each year from 2018 to 2022. Thus, the implementation of restrictions for TB-suspected and TB-positive patients on regular basis can help prevent the spread of the disease.
Acknowledgement
We are thankful to the Department of Pulmonary Medicine, General Medicine and Pediatrics for sending samples to us. We are thankful to our technicians Pankaj Ade, Swati Dixit, and Pramod Bhalchim for carrying out the tests and maintaining an appropriate turnaround time for TB testing even during the COVID-19 period.
Funding sources
None.
Ethical statement
Ethical approval was taken with reference number 1023291-291(Dated 27/10/2023)
Conflicts of interest
The authors declare no conflict of interest.
Author contributions
SSP: Conceived the idea and revised the manuscript; PGS: Drafted the manuscript; VVG, SND, MVR, RPK: Reviewed the manuscript. All authors read and approved the final manuscript.
Data availability statement
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
Full-Text: (335 Views)
Introduction
India contributes almost a quarter of the global Tuberculosis (TB) burden (1). It is the second most common cause of death among infectious diseases (2). The silent epidemic of TB was overshadowed by the COVID-19 pandemic which began in March 2020, and majorly continued till January 2022 and a few cases have been found to date. The focus in the years 2020 to 2021 was completely on COVID-19. The peak of the first wave of the pandemic was in mid-September when there were more than one million active cases in the country, with the highest single-day spike of 97,894 new cases recorded on September 16, 2020 (3). By the end of February 2021, there was a sharp rise in the number of daily reported cases, which culminated in the second wave of the pandemic (4). The third wave began in December 2021 and remained up to January 2022. The pandemic continues and a few cases have been found to date. Since COVID-19 and TB are the diseases of respiratory system, they might have an impact on each other. Having a reliable estimate of the association between TB and COVID-19 severity and mortality is crucial to ensure specific successful global preventive and treatment strategies for patients with TB (5). When a patient suffers from a previous respiratory disease, the patient's lung function is impaired and their resistance to viruses is low and they tend to develop acute respiratory distress syndrome (6). Both pathogens may lead to an unbalanced inflammatory immune response, and together a shared dysregulation of immune response suggests an increased risk of severity and progression of both diseases (7). This study was mainly conducted to assess the impact of COVID-19 on TB whether the cases have raised or have fallen in the pandemic period. This study was also conducted to investigate whether the isolation, lockdown, strict quarantine measures taken for COVID-19 were effective for TB. The aim of the present study was to detect Mycobacterium tuberculosis (M. tuberculosis) and rifampicin resistance before, during, and after COVID-19 restrictions were fully released.
Methods
This was a five-year retrospective study conducted at a tertiary care hospital from 1st January 2018 to 31st December 2022. The study period was divided into three phases: the COVID-19–free period (January 2018 to February 2020), the COVID-19 period with restrictions (March 2020 to June 2021), and the COVID-19 period without restrictions (July 2021 to December 2022) (8,9). The inclusion criteria were patients of all age groups and gender clinically suspected to have TB irrespective of any co-morbid condition and drug history. Exclusion criteria were samples received for tests other than TB. The study procedure was as follows: Early morning deeply expectorated samples were collected from clinically suspected cases of TB. They were taken in sterile wide-mouth containers after obtaining consent from the patient. Extrapulmonary samples were collected depending on the site. The samples were subjected to GeneXpert MTB/RIF manufactured by Cepheid, France for detection of M. tuberculosis and rifampicin resistance in them. They were processed according to the manufacturer’s guidelines. A p-value of less than 0.05 was considered statistically significant.
Results
The total samples received for M. tuberculosis from 2018-2022 were 3543, 3823, 3682, 3248, and 3381 respectively. The total number of pulmonary and extra-pulmonary samples are summarized in Table 1. This study was mainly conducted to see the impact of COVID-19 on TB. We found that the positivity for M. tuberculosis was 20.9%, 18.2%, 15.5%, 15.8%, and 16.8% from 2018 to 2022, respectively (Table 2). The rifampicin resistance detected during the same years was 11.0%, 9.8%, 7.3%, 6.4%, and 11.9%, respectively (Table 2). This result was found to be statistically significant (p = 0.042). M. tuberculosis detection from extrapulmonary samples was minimum (11.58%) in 2020 which increased in later years (Table 3). No significant change in rifampicin resistance was noted for extrapulmonary samples.
Table 2 indicates decreased positivity and rifampicin resistance in 2020 and 2021. p-value= 0.042 which was statistically significant.
India contributes almost a quarter of the global Tuberculosis (TB) burden (1). It is the second most common cause of death among infectious diseases (2). The silent epidemic of TB was overshadowed by the COVID-19 pandemic which began in March 2020, and majorly continued till January 2022 and a few cases have been found to date. The focus in the years 2020 to 2021 was completely on COVID-19. The peak of the first wave of the pandemic was in mid-September when there were more than one million active cases in the country, with the highest single-day spike of 97,894 new cases recorded on September 16, 2020 (3). By the end of February 2021, there was a sharp rise in the number of daily reported cases, which culminated in the second wave of the pandemic (4). The third wave began in December 2021 and remained up to January 2022. The pandemic continues and a few cases have been found to date. Since COVID-19 and TB are the diseases of respiratory system, they might have an impact on each other. Having a reliable estimate of the association between TB and COVID-19 severity and mortality is crucial to ensure specific successful global preventive and treatment strategies for patients with TB (5). When a patient suffers from a previous respiratory disease, the patient's lung function is impaired and their resistance to viruses is low and they tend to develop acute respiratory distress syndrome (6). Both pathogens may lead to an unbalanced inflammatory immune response, and together a shared dysregulation of immune response suggests an increased risk of severity and progression of both diseases (7). This study was mainly conducted to assess the impact of COVID-19 on TB whether the cases have raised or have fallen in the pandemic period. This study was also conducted to investigate whether the isolation, lockdown, strict quarantine measures taken for COVID-19 were effective for TB. The aim of the present study was to detect Mycobacterium tuberculosis (M. tuberculosis) and rifampicin resistance before, during, and after COVID-19 restrictions were fully released.
Methods
This was a five-year retrospective study conducted at a tertiary care hospital from 1st January 2018 to 31st December 2022. The study period was divided into three phases: the COVID-19–free period (January 2018 to February 2020), the COVID-19 period with restrictions (March 2020 to June 2021), and the COVID-19 period without restrictions (July 2021 to December 2022) (8,9). The inclusion criteria were patients of all age groups and gender clinically suspected to have TB irrespective of any co-morbid condition and drug history. Exclusion criteria were samples received for tests other than TB. The study procedure was as follows: Early morning deeply expectorated samples were collected from clinically suspected cases of TB. They were taken in sterile wide-mouth containers after obtaining consent from the patient. Extrapulmonary samples were collected depending on the site. The samples were subjected to GeneXpert MTB/RIF manufactured by Cepheid, France for detection of M. tuberculosis and rifampicin resistance in them. They were processed according to the manufacturer’s guidelines. A p-value of less than 0.05 was considered statistically significant.
Results
The total samples received for M. tuberculosis from 2018-2022 were 3543, 3823, 3682, 3248, and 3381 respectively. The total number of pulmonary and extra-pulmonary samples are summarized in Table 1. This study was mainly conducted to see the impact of COVID-19 on TB. We found that the positivity for M. tuberculosis was 20.9%, 18.2%, 15.5%, 15.8%, and 16.8% from 2018 to 2022, respectively (Table 2). The rifampicin resistance detected during the same years was 11.0%, 9.8%, 7.3%, 6.4%, and 11.9%, respectively (Table 2). This result was found to be statistically significant (p = 0.042). M. tuberculosis detection from extrapulmonary samples was minimum (11.58%) in 2020 which increased in later years (Table 3). No significant change in rifampicin resistance was noted for extrapulmonary samples.
Table 2 indicates decreased positivity and rifampicin resistance in 2020 and 2021. p-value= 0.042 which was statistically significant.
Table 1. Total samples received from 2018 to 2022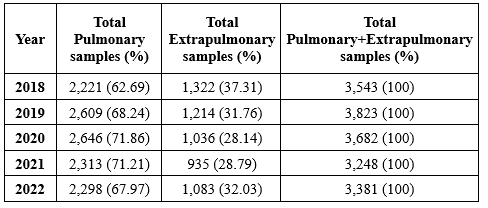 Table 2. Year-wise distribution of samples received, samples positive for Mycobacterium tuberculosis and rifampicin resistance by CBNAAT 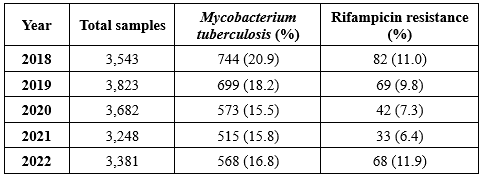 Table 3. Total extrapulmonary samples, positive and negative for M. tuberculosis from 2018 to 2022 .PNG) |
Discussion
This study was conducted in a tertiary care hospital from 1st January 2018 to 31st December 2022. The total samples received for M. tuberculosis from 2018-2022 were 3543, 3823, 3682, 3248, and 3381 respectively. Samples positive for M. tuberculosis were 20.9%, 18.2%, 15.5%, 15.8%, and 16.8% from 2018 to 2022, respectively. The rifampicin resistance from 2018 to 2022 was found to be 11.0%, 9.8%, 7.3%, 6.4%, and 11.9%, respectively. During the study period, two years i.e., 2020 and 2021 were the COVID-19 pandemic period in India. Moreover, many restrictions were imposed to stop the spread of COVID-19 during these years, such as wearing masks, avoiding social gatherings, maintaining social distancing, etc., which are all isolation measures. It was observed that the positivity of TB in our tertiary care hospital decreased in 2020 and 2021. The rifampicin resistance also decreased during the same period.
In the present study, the years 2018 and 2019 can be considered the pre-COVID-19 period, while the year 2022 was considered the COVID-19 period without restrictions. M. tuberculosis positivity and rifampicin resistance were higher in the pre-COVID-19 (22.5%) and post-COVID-19 (16.8%) periods compared to the COVID-19 period with restrictions (15.7%). Tuberculosis and COVID-19 are diseases of the respiratory system and they spread through droplet nuclei (10). Isolation measures followed during COVID-19 might contribute to decreasing cases of TB during 2020 and 2021.
The importance of masks in the prevention of airborne diseases has been mentioned by CDC and Asadi et al. (11,12). Moreover, the lockdowns likely had a significant impact, as fear of COVID-19 led people to minimize contact even with family members. This reduction in interaction may have helped prevent the spread of infection within households and the broader community. Afterward, vaccination was introduced widely in India. In 2021, India reported around 1.6 lakhs vaccination every hour (12). At the same time, cases of COVID-19 started decreasing and restrictions were partially released. In 2022, the milder omicron wave was documented; however, strict restrictions were not imposed again. This could be the major reason for the increase in cases in 2022. In the study conducted by Miligori et al., TB decreased from 32,898 (Mean±SD=2742±177 per month) in 2019 to 16,396 (1366±308 per month; p<0.0001) in 2020, with a sudden decline in March 2020, concomitantly with the commencement of lockdown in the majority of the countries (13). This epidemiological change was observed in all countries, except TB centers in Australia, Singapore, and Virginia (13).
In the present study, the lowest rifampicin resistance was seen in 2021. The possible reason could be lockdown restricted movement of people and social gatherings. As a result, many people may not have accessed diagnostic facilities, leading to underreporting of rifampicin resistance. In the study conducted by Trajman A. et al., the COVID-19 pandemic had a sufficient impact on TB care cascade, resulting in decrease in TB testing and notifications of TB, primarily as a result of disrupted TB services and constrained patient movement (14). However, restrictions were released, and an increase was reported in rifampicin resistance in 2022.
Extrapulmonary TB-positive cases were not seen to decrease significantly during the COVID-19 period. In fact, we observed an increase in the number of TB-positive cases from extrapulmonary samples in 2021. This clearly indicates that wearing masks has prevented only pulmonary TB. As very few studies are available on TB in the COVID-19 period, we could not compare our results with similar studies.
In case of rifampicin-resistant TB, we could not track family members of rifampicin-resistant patients to confirm their rifampicin status. These findings cannot be generalized, since this is a single-center study. Further studies, especially in bigger institutes will enable us to know the overall status and can be useful to take further action. There is a need to conduct a cohort study on people who wear masks and those who do not.
Conclusion
Restrictions imposed during the COVID-19 period could have decreased TB as well as rifampicin resistance. There was not much difference in total sample size received each year from 2018 to 2022. Thus, the implementation of restrictions for TB-suspected and TB-positive patients on regular basis can help prevent the spread of the disease.
Acknowledgement
We are thankful to the Department of Pulmonary Medicine, General Medicine and Pediatrics for sending samples to us. We are thankful to our technicians Pankaj Ade, Swati Dixit, and Pramod Bhalchim for carrying out the tests and maintaining an appropriate turnaround time for TB testing even during the COVID-19 period.
Funding sources
None.
Ethical statement
Ethical approval was taken with reference number 1023291-291(Dated 27/10/2023)
Conflicts of interest
The authors declare no conflict of interest.
Author contributions
SSP: Conceived the idea and revised the manuscript; PGS: Drafted the manuscript; VVG, SND, MVR, RPK: Reviewed the manuscript. All authors read and approved the final manuscript.
Data availability statement
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
Research Article: Original Paper |
Subject:
Microbiology
Received: 2024/07/24 | Accepted: 2024/12/31 | Published: 2025/01/29 | ePublished: 2025/01/29
Received: 2024/07/24 | Accepted: 2024/12/31 | Published: 2025/01/29 | ePublished: 2025/01/29
References
1. Sathiyamoorthy R, Kalaivani M, Aggarwal P, Gupta SK. Prevalence of pulmonary tuberculosis in India:A systematic review and meta-analysis. Lung India. 2020; 37: 45-52. [View at Publisher] [DOI] [PMID] [Google Scholar]
2. World Health Organisation. Global Tuberculosis Control Report 2011. . 2011. [View at Publisher]
3. Press Information Bureau Government of India Ministry of Health and Family Welfare. India records more than 82,000 Recoveries for two days in a row. 2021. [View at Publisher]
4. Agarwala P, Bhargava A, Gahwai DK, Negi SS, Shukla P, Dayama S. Epidemiological Characteristics of the COVID-19 Pandemic During the First and Second Waves in Chhattisgarh, Central India: A Comparative Analysis. Cureus. 2022; 14(4):e24131. [View at Publisher] [DOI] [PMID] [Google Scholar]
5. Gao Y, Liu M, Chen Y, Shi S, Geng J, Tian J. Association between tuberculosis and COVID-19 severity and mortality: A rapid systematic review and meta-analysis. J Med Virol.2021; 93(1): 194-196. [View at Publisher] [DOI] [PMID] [Google Scholar]
6. Zheng Z, Peng F, Xu B. Risk factors of critical & mortal COVID‐19 cases: a systematic literature review and meta‐analysis. J Infect. 2020; 10. [View at Publisher] [DOI] [PMID] [Google Scholar]
7. Luke E, Swafford K, Shirazi G, Venketaraman V. TB and COVID-19: An Exploration of the Characteristics and Resulting Complications of Co-infection. Front Biosci (Schol Ed). 2022; 14(1): 6. [View at Publisher] [DOI] [PMID] [Google Scholar]
8. Rai B, Shukla A, Dwivedi L K. Dynamics of COVID-19 in India: A review of different phases of lockdown. Population Medicine. 2020; 2(July): 21. [View at Publisher] [DOI] [Google Scholar]
9. Wikipedia. Covid-19 lockdown in India. 2023. [View at Publisher]
10. Hopewell PC, Reichman LB, Castro KG. Parallels and Mutual Lessons in Tuberculosis and COVID-19 Transmission, Prevention, and Control. Emerg Infect Dis. 2021; 27(3): 681-686. [View at Publisher] [DOI] [PMID] [Google Scholar]
11. Asadi S, Cappa CD, Barreda S, Wexler AS, Bouvier NM, Ristenpart WD. Efficacy of masks and face coverings in controlling outward aerosol particle emission from expiratory activities. Sci Rep. 2020; 10: 1566. [View at Publisher] [DOI] [PMID] [Google Scholar]
12. the times of india. Devastating 2nd wave, billion+ vaccination: 12 charts show how india fought covid in 2021. 2022. [View at Publisher]
13. Migliori GB, Thong PM, Alffenaar J-W. Gauging the impact of the COVID-19 pandemic on tuberculosis services: a global study. EurRespir J. 2021; 58: 2101786. [View at Publisher] [DOI] [PMID] [Google Scholar]
14. Trajman A, Felker I, Alves LC, Coutinho I, Osman N, Meehan SA, et al. The COVID-19 and TB syndemic: The way forward. International J of Tuberculosis and lung disease. 2022; 26(8): 710-719. [View at Publisher] [DOI] [PMID] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.




 goums.ac.ir
goums.ac.ir yahoo.com
yahoo.com